Material below is adapted from the SfN Short Course Probing Disorders of the Nervous System Using Reprogramming Approaches, by Evangelos Kiskinis, PhD. Short Courses are day-long scientific trainings on emerging neuroscience topics and research techniques held the day before SfN’s annual meeting.
While animal models provide important insights into neurological disease, they rarely offer a complete picture: Findings sometimes fail to translate to humans and animal models often don’t mirror how neurological diseases develop and progress in humans. Neuroscience researchers need experimental systems that accurately mimic the genetic background, environment, and variability seen in humans.
One promising method for addressing this problem involves reprogramming cells from patients to become stem cells or even specific neuronal cell types. These reprogrammed cells provide new avenues for drug discovery and the development of patient-specific treatments.
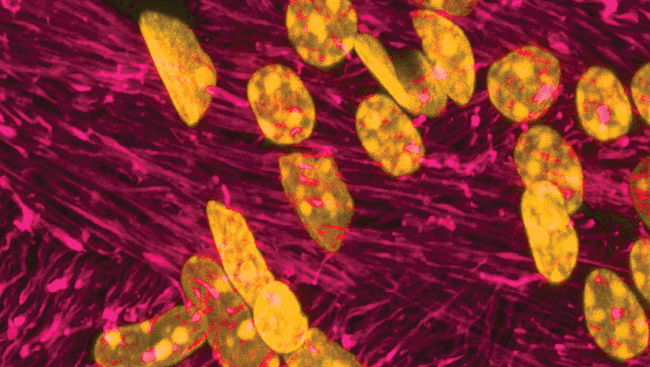
Known as induced pluripotent stem cells (iPSCs), these reprogrammed cells possess the potential to become any cell type. Scientists create them by exposing adult cells such as skin fibroblasts or blood mononuclear cells to a cocktail of chemical cues that revert the cell to a pluripotent stem-cell-like state. Other factors can nudge the cells to develop into specific cell subtypes vulnerable to disease. This type of cellular reprogramming now allows researchers to model and characterize the heterogeneity of diseases as seen in real patient populations.
Researchers first produced such cells to confirm that the induced neurons could recapitulate such conditions as Amyotrophic Lateral Sclerosis (ALS), Alzheimer's disease, and autism. The next wave of studies with iPSCs unraveled how these diseases develop and progress. Still, recent studies show generating effective control cell lines to match the iPSC lines remains a challenge.
A new, targeted genetic technology called CRISPR/Cas9 may provide a solution by allowing researchers to precisely cut DNA strands and introduce the desired genetic alterations. Using CRISPR/Cas9 technology, researchers can modify an iPSC line to provide its own control. Generating multiple stem cell clones from each patient, a step that makes clear which observed differences are due to errors in the clonal cell line and which are due to the disease, is another way to reduce experimental variation.
In order to study how disease progression, researchers must propagate the type of cell that will show a disease's effects. This may involve first developing the correct neural cell type, and, then, maturing that cell so that age-related disease phenotypes — such as those in Huntington's disease, Alzheimer's disease, or Parkinson's disease — develop. Researchers continue to explore exactly which chemical cues age iPSC cells.
Growing cells in the correct environment is also key to understanding how disease develops in the body. As useful as cell culture is, the milieu of liquid, nutrients, and growth factors does not mimic the structure and functional networks of the nervous system. Researchers have made strides in developing cultures where multiple cell types grow together and influence each other — for example, spinal motor neurons have been co-cultured with cortical astrocytes in a model of ALS. Another approach involves growing miniature structures that resemble the three-dimensional structure of brain tissue. These so-called organoids can even recapitulate the organization of brain regions. Not all experiments with such systems have included iPSCs, but it is an area ripe for exploration.