Material below summarizes the article Microglia Play an Active Role in Obesity-Associated Cognitive Decline, published on October 10, 2018, in JNeurosci and authored by Elise C. Cope, Elizabeth A. LaMarca, Patrick K. Monari, Lyra B. Olson, Susana Martinez, Anna D. Zych, Nicole J. Katchur and Elizabeth Gould.
The World Health Organization has labeled obesity a global epidemic with major public health implications.
In humans, obesity produces many well-known health challenges, but one lesser-known danger is it diminishes cognitive function. Obesity also predisposes individuals to develop serious cognitive disorders later in life, such as dementia and Alzheimer's disease.
Neuroimaging studies have shown reduced brain volume in obese humans, particularly in areas that support cognitive function. Yet, the cellular processes underlying the association between obesity and neuronal structure remain elusive.
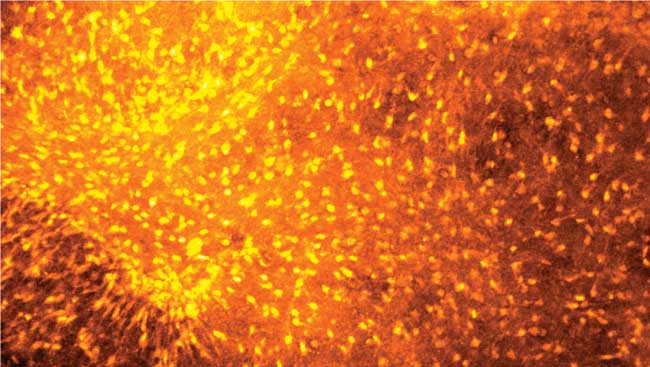
Studies have shown obese rodents have fewer-than-normal synapses in the hippocampus and prefrontal cortex, two areas important for cognitive function. Reduced synaptic connections coincide with changes in microglial morphology in these brain regions in obese rodents. Microglia are the immune cells of the brain, and one of their main functions is to clean up neuronal debris. An obvious interpretation of the literature is microglia help clean up the remains of synaptic connections after those connections have been destroyed.
However, accumulating evidence suggests microglia also shape brain circuits by engulfing weak synapses during development, a process known as synaptic pruning. We hypothesized something similar might be happening in the obese brain, but at a pathological level. In this way, we predicted, microglial malfunction might be directly responsible for synapse loss, resulting in cognitive decline associated with obesity.
To address this, we used high-fat or high-sugar diets to induce obesity in adult male mice. Consistent with previous studies, we found cognitive impairments on tests of hippocampal function, along with reduced numbers of dendritic spines (sites of synapses) on hippocampal neurons.
We also found increases in microglial reactivity, such as altered microglial morphology and increases in CD68 (a marker of microglial phagocytosis), as well as evidence of internalized synaptic components within microglia in the hippocampus of obese mice.
We then asked whether we could block microglia to improve behavioral outcomes and neural structure in obese mice.
Partial transgenic ablation of the microglial receptor for fractalkine, a signal that serves as a “find me” cue to attract microglia to dying neurons, prevented cognitive decline and microglial reactivity in obese mice. In addition, the antibiotic drug minocycline, which blocks microglial reactivity, improved the performance of obese mice on cognitive tests and increased the number of dendritic spines on hippocampal neurons.
Although these data suggest microglia are actively involved in synapse elimination and resulting cognitive decline associated with obesity, they do not provide information as to a mechanism. Since microglia release several inflammatory molecules that can be damaging to neuronal structure, one interpretation of our findings is microglia first render synapses nonfunctional and then only secondarily engulf the synaptic debris.
To eliminate this possibility and test the hypothesis that microglia eliminate synapses by overeating healthy connections, we treated obese mice with a drug to inhibit microglial engulfment, annexin-V, which blocks an “eat me” signal exposed by dying cells and synapses.
In addition to having fewer engulfed synaptic components within microglia, obese mice treated with annexin-V performed as well as control mice did on cognitive tests. This suggests cognitive decline resulted from microglia engulfing synaptic connections excessively in the obese brain.
Collectively, our studies suggest that microglia malfunction and overeat healthy synapses in the obese brain, which leads to cognitive decline.
Still remaining is the question of what triggers microglia to malfunction in the first place.
In our study, we exposed mice to a high-fat or -sugar diet for long durations, both producing cognitive impairment. We also exposed mice to either of these diets for short durations, which did not result in increased fat mass or body weight.
These mice had normal cognitive function with no changes in microglia, suggesting there is something specific about fat tissue that disrupts microglial function. Because fat tissue acts a neuroendocrine organ to release inflammatory molecules, it may signal microglia to malfunction and begin overeating healthy synaptic connections. Over time, the brain shrinks as microglia deplete healthy neural connections, resulting in cognitive impairment associated with obesity.
Fortunately, our data show the negative impacts of obesity on brain structure and function are reversible with treatments that block microglial function. It’s also likely lifestyle changes such as weight loss and increased physical activity would mitigate some of the detrimental effects of obesity on cognition.
Broader implications of our work extend to neurodegenerative conditions, which are associated with cognitive impairment and immune dysfunction.
Visit JNeurosci to read the original article and explore other content. Read other summaries of JNeurosci and eNeuro papers in the Neuronline collection SfN Journals: Research Article Summaries.
Microglia Play an Active Role in Obesity-Associated Cognitive Decline. Elise C. Cope, Elizabeth A. LaMarca, Patrick K. Monari, Lyra B. Olson, Susana Martinez, Anna D. Zych, Nicole J. Katchur and Elizabeth Gould. JNeurosci Oct 2018, 38 (41) 8889–8904; DOI: 10.1523/JNEUROSCI.0789-18.2018