Material below is adapted from the SfN Short Course Alzheimer’s Disease Genetics: From the Bench to the Clinic, by Celeste M. Karch, PhD, Carlos Cruchaga, PhD, and Alison Goate, DPhil. Short Courses are daylong scientific trainings on emerging neuroscience topics and research techniques held the day before SfN’s annual meeting.
The symptoms characterizing Alzheimer’s disease — memory loss and general cognitive decline — appear to derive from physical changes within the brain including amyloid plaque accumulation in the extracellular spaces, tangled fibrils of tau proteins within neural cells, and gross atrophy.
Genetic studies indicate specific mutations cause or increase the risk of Alzheimer’s disease. These discoveries help illuminate some of the biological missteps leading to disease. With the advent of newer techniques and falling costs, particularly for genotyping and sequencing, scientists are beginning to identify additional genetic components of the disease.
Evidence for a genetic component to Alzheimer’s disease was initially found in families in which multiple members developed the disorder, often in middle age. Researchers targeted this early-onset, familial form seeking to link specific genetic changes to increased risk by comparing sequences of specific genes of family members with and without the disease.
As a result of numerous studies, researchers identified mutations in three genes capable of causing Alzheimer’s disease. Amyloid precursor protein (APP) can be cleaved into a variety of smaller fragments, some of them harmful. One fragment, amyloid beta, tends to clump to form plaques, and mutations of the gene for APP that favor the production of amyloid beta cause Alzheimer’s disease. Accumulation of amyloid in the extracellular spaces is believed to trigger additional pathological changes in the brain.
Genetic linkage studies have also pinpointed alterations in the enzymes that cleave APP as a cause of Alzheimer’s disease, either by increasing the amount of amyloid beta or by altering the ratio of two different forms of amyloid beta. Mutations in the genes PSEN1 or PSEN2, produce these malfunctioning enzymes.
A fourth gene, for apolipoprotein E (APOE), shifts the risk of Alzheimer’s disease. Most people carry an APOE allele associated with average risk for the disease. Genetic linkages studies have identified two more alleles, one that increases risk for the disease eight o 10 fold and one that seems protective. APOE serves a variety of biological processes but among them is the aggregation and clearance of amyloid beta.
Only half of the people with Alzheimer’s carry the high-risk APOE allele and just two percent carry one of the other causal mutations. The availability of relatively inexpensive genotyping has allowed researchers to expand the search for other genetic risk factors to thousands of patients.
Genome-wide association studies identify genetic regions, or loci, associated with elevated risk of disease, and scientists have found 20 such loci so far. They are still working out exactly which genes are involved, but many genes in and near loci identified with risk have a putative immune function suggesting that inflammation may play a role.
Additional genetic risk factors may emerge as the populations screened continue to increase and widen beyond people of European descent, and as researchers broaden the phenotypes considered to include other measures such as the rate of disease progression, rate of cognitive decline, and age at onset of symptoms.
By analyzing the networks of regulatory pathways scientists have identified one potential key regulatory protein — a protein influencing the activity of genes — that spurs the development of Alzheimer’s disease.
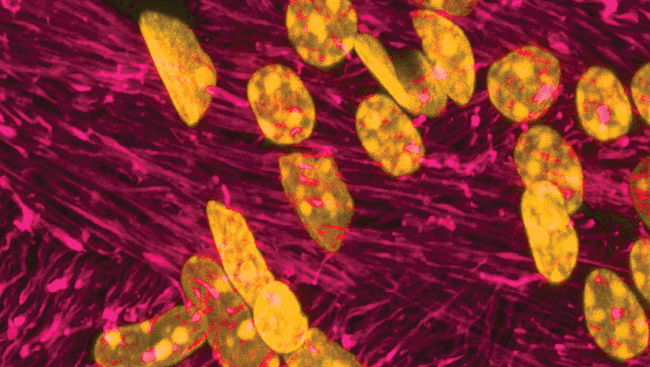
Genome-wide association studies routinely miss contributions of rare alleles because they rely on chips designed to capture only relatively common genetic variants. In order to address that pitfall, the use of sequencing whole-genomes and whole-exomes has grown to encompass thousands of individuals. In one early success of the strategy, two groups independently identified a mutation of TREM2 that doubles or triples the risk of Alzheimer’s disease. TREM2 is expressed in microglia, the immune cells of the brain, which fail to cluster around amyloid plaques in a mouse model of the harmful mutation.
Genome and exome sequences and results from genome-wide association studies are being collected into public databases such as the National Library of Medicine’s Database of Genotypes and Phenotypes, providing a rich and public resource for teasing out the genetic contributions and potential treatments for this and likely other devastating neurodegenerative diseases.