Why This Researcher Studies Mitochondria
- Featured in:
- Neurobiology of Disease Workshops
Phillip West is an assistant professor of microbial pathogenesis and immunology at the Texas A&M University Health Science Center. He led a breakout group at the 2016 Neurobiology of Disease Workshop, From Pediatric Encephalopathy to Alzheimer's: Linking Mitochondria to Neurological Diseases, and presented in 2017 follow-up webinar, Linking Mitochondria to Neurological Disease. Here, he shares what led him to this research path and why it excites him. As told to, and edited by, SfN staff.
“I stumbled into the area of mitochondria, and it turned out to be serendipitous.
While doing my PhD in immunobiology in Sankar Ghosh’s Lab at Yale, I started working on a protein, ECSIT (Evolutionarily Conserved Signaling Intermediate in Toll Pathways), that had been cloned in the Ghosh lab a few years before I arrived.
My project focused on characterizing the cell biology of this protein and understanding where it was localized and how it influenced NF-kappaB signaling.
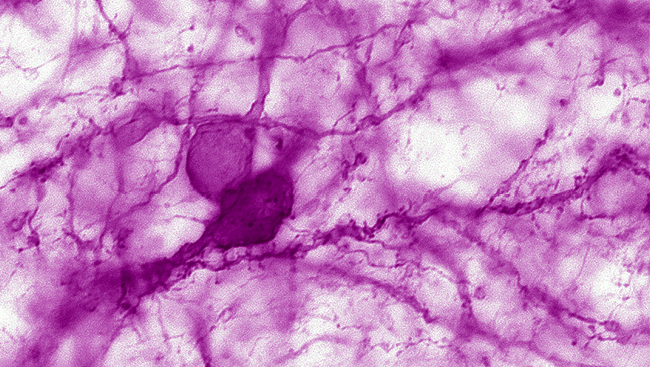
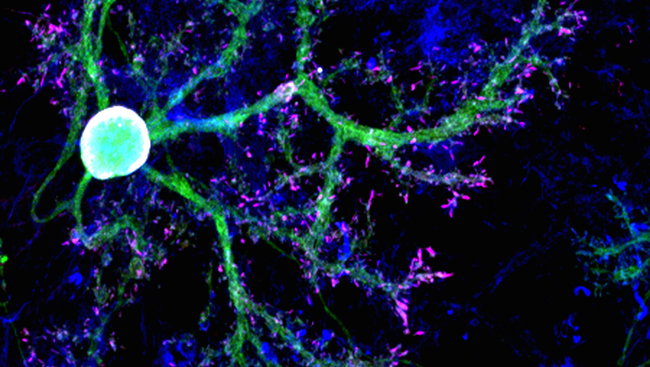
About three years into my PhD, I noticed that any time we performed immunostaining (staining cells with antibodies to look at where the protein was localized), there was always a very punctate or tubular pattern, which I found interesting.
Knowing nothing about mitochondria and not a lot about cell biology at that time, I found a collaborator in Yale’s cell biology department. This individual told me that these punctate patterns were mitochondria.
That completely stunned me, because up until that point, we thought ECSIT was a cytosolic protein.
This new piece of information changed the entire concept I was working on, so I rewrote my thesis aims.
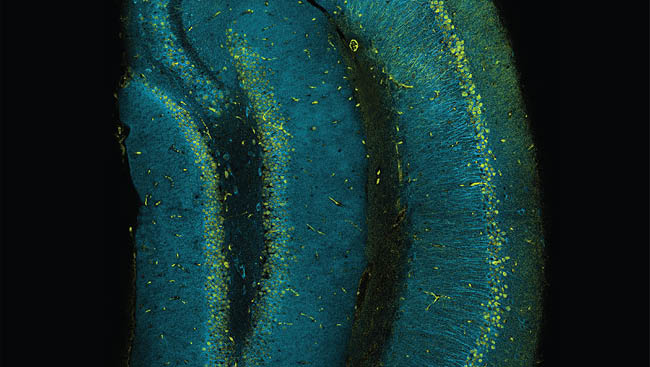
After this discovery, I began reading and learning about mitochondria, which are organelles found in most of the cells in our body. I thought that it was an awesome opportunity to learn something new about an area of biology I really know very little about.
I also started working with Gerry Shadel, a mitochondrial biologist at Yale. He helped me think about how this protein might be functioning in mitochondria.
I spent three more years on that project. We then published a paper in Nature detailing how the ECSIT protein regulates reactive oxygen species production from mitochondria, and how that influences immune responses against bacteria.
Around that time, mitochondrial biology was undergoing a rebirth, as it was becoming clear that mitochondria impacted many human diseases and aging. I stayed in Gerry Shadel’s lab at Yale for my postdoctoral fellowship and investigated how mitochondria regulate innate immunity and cancer.
Currently, the focus of my research is to better understand how mitochondrial dysfunction regulates the immunopathology of various diseases.
In other words, we’re looking at how mitochondria regulate innate immune responses and investigating how those responses and associated inflammation can impact a variety of diseases.
The innate immune response is the first line of defense against pathogens. It senses viral, bacterial, and fungal pathogens, alerting the body that there is a problem.
In approximately the past 10 years, it’s come out that mitochondria sit at the center of many innate immune responses. Signals are transited across mitochondria, and the mitochondria then recruit factors and pass signals downstream to change gene expression, thereby influencing the outcome of an immune response.
Mitochondria are also dysfunctional in many diseases. They don't move to the same degree. They don't generate the same level of energy. They have a variety of impaired metabolic pathways.
In addition, when the integrity of mitochondria is compromised or there is some breakdown in the ability to clean up damaged mitochondria, the damaged mitochondria can accumulate and release molecules into the host's cytoplasm or outside of cells that look like foreign molecules.
When these molecules enter the cytoplasm or the extra-cellular space, they can trigger innate immune responses.
To understand how mitochondria regulate like physiological innate immune responses, my lab is looking at several disease models, including Gulf War Illness, cancer, and mitochondrial diseases.
Besides the questions that my lab is pursuing, there are a few other reasons why mitochondrial research is exciting to me.
What’s most intriguing are the evolutionary underpinnings. Mitochondria have essentially co-evolved with the host to shape different immune responses, almost as if the host says, "Okay, well we've incorporated you. You're great at making energy, but why don't we also give you additional roles in regulating immune responses?"
Also really exciting is the work from Xinnan Wang, Heidi McBride, and Richard Youle, who I joined for the 2016 Neurobiology of Disease Workshop and related 2017 follow-up webinar. They have blown the top off of studying the way mitochondria move in cells and how that movement regulates their function.
Additionally, the diversity of techniques that we use keeps me engaged. When you study mitochondrial biology, you're always refreshing your technique base.
The field is also great because you can always tether mitochondria to anything. In a funding climate like we have, it's nice to study something that's relevant to so many diseases.
There's certainly a debate about whether mitochondrial dysfunction is a driver of disease or just a symptom of disease — the chicken and egg question. But given that mitochondrial function and dysfunction are so important in different diseases, mitochondrial researchers can broaden quickly beyond their comfort zone.
While there are a lot of observations being made about mitochondria regulating immune responses, there are still gaps in our understanding of how this happens. I hope that in the future unifying themes will tie these observations together.
I also hope that we'll have better techniques and methodologies to monitor mitochondrial triggering of immune responses and inflammation in real time.
I'm a basic research scientist, but I'm always trying to think about how my research is relevant to human disease and if there any targetable approaches.
Hopefully, the field will move us ahead enough that if we understand how to target mitochondrial driven immune responses, we'll be able to selectively target the bad ones and limit immunopathology in different diseases.
Perhaps then we can therapeutically intervene and improve the health of people suffering from these conditions.”
Watch the 2016 Neurobiology of Disease Workshop, From Pediatric Encephalopathy to Alzheimer's: Linking Mitochondria to Neurological Diseases, and the 2017 follow-up webinar, Linking Mitochondria to Neurological Disease.
Speaker